Cycologist
In my last blog, I ruminated on developing hip osteoarthritis (OA) and the impact of living with OA, in particular its impact on my lifelong passion for running. I have adapted and over the summer, I became a cycologist (an alluring new kind of cerebral nuance on cyclist that I saw on a t-shirt with an obvious pun on psychologist) sporting a new electric assist bicycle, this one:

It is a Gazelle Ultimate C80 53cm, Sienna Light in colour. In late June, it was mostly assembled and shipped from a company called Citrus Cycles in Chemainus, British Columbia. Behind it, on the wall is a shelf I built for the battery charger, the battery itself housed in the black section of the diagonal structure between the two wheels on the bike. My C80 came in this cardboard container:

All I had to do was reposition and tighten the front handlebars and screw in the pedals (reverse thread on the left pedal or else pedalling action might unscrew the pedal, who knew). Our eldest son, Matt recommended the bike model to me. He sells e-bikes in Hood River, Oregon and he thought was this would be perfect model for me…and it is. No bike derailleur – I know nothing about bikes and derailleurs so wanted something that did not have high or technical maintenance issues. The chain cannot come off and lasts for about 10 years. All I have needed so far is some Allen wrenches or keys, a multi-tool set of which another of our sons, Joe (triathlete, avid cyclist) gave me for my birthday and a torque wrench for making sure any adjustments to various nuts are not over-or under-tightened. Learning to use the torque wrench was novel and I think I have acquired the torque technique. Matt also supplemented his expertise with a generous gift certificate to a local bike store, London Bicycle Cafe from where I bought my helmet, side-mirrors, and front pack:

The front pack carries my phone, packaged N95 masks, wrench set, and an address ID tag with Jen’s phone number. From my motorcycle riding days, I am accustomed to having side-view mirrors and consider them essential to the kind of touring style of riding I do. The brakes are disc ones, so really good quality and I replaced the original bell with one of higher and more audible pitch. On all rides, I turn on front and rear lights and my helmet even has a battery-powered triangular light on the back…not so visible in bright light but discernible when overcast or dark. Very quickly, I learned riding necessitated much more padding on the seat, or my seat than regular clothing. Thus, I now own gel-padded shorts and gel-padded, reflective tights, and more recently, a wind-water-proof jacket and balaclava, the latter two essential for Fall rides in cooler weather.
Very unexpectedly, I can honestly say, I love riding my electric assist bike. One of the keys to e-bike riding is the handlebar-mounted computer:
 This device is located easily within reach of my left-hand fingers; its display enables me to see important information like my speed, distance travelled, battery range remaining, and most importantly, my selected motor assistance level and I assume it is powered from the main bike battery. Pressing the top button turns the unit on; then, holding the plus button visible on the side for a few seconds turns on the front and rear lights. I can set the display in various ways and the image shows my preferences – speed in km/hour on the top; cumulative distance travelled in km; and the 4 little bars inside the battery outline show the amount of battery charge left before re-charging is needed, so far about every 100 km. This unit also controls the 4 levels of e-assistance needed, from Eco (lowest) to Tour, to Sport, to Turbo (highest). The minus button is to go to a lower e-assist level and the bike can be ridden without any e-assistance. The Gazelle will not engage any e-assistance level on its own; the rider has to select and change the level as needed and the assistance is only related to pedalling. All of this was very new to me as was the gear shifting; eight gears selected by moving a knob on the inside edge of the right handle grip. Using the gears has taken the most conscious learning because on motorcycles, I was accustomed to shifting by engaging the clutch via what is one of the brake levers on my Gazelle and then changing gears with my left foot, kind of hard-wired after so many years of riding motorcycles.
This device is located easily within reach of my left-hand fingers; its display enables me to see important information like my speed, distance travelled, battery range remaining, and most importantly, my selected motor assistance level and I assume it is powered from the main bike battery. Pressing the top button turns the unit on; then, holding the plus button visible on the side for a few seconds turns on the front and rear lights. I can set the display in various ways and the image shows my preferences – speed in km/hour on the top; cumulative distance travelled in km; and the 4 little bars inside the battery outline show the amount of battery charge left before re-charging is needed, so far about every 100 km. This unit also controls the 4 levels of e-assistance needed, from Eco (lowest) to Tour, to Sport, to Turbo (highest). The minus button is to go to a lower e-assist level and the bike can be ridden without any e-assistance. The Gazelle will not engage any e-assistance level on its own; the rider has to select and change the level as needed and the assistance is only related to pedalling. All of this was very new to me as was the gear shifting; eight gears selected by moving a knob on the inside edge of the right handle grip. Using the gears has taken the most conscious learning because on motorcycles, I was accustomed to shifting by engaging the clutch via what is one of the brake levers on my Gazelle and then changing gears with my left foot, kind of hard-wired after so many years of riding motorcycles.
My vision for getting the e-bike was to be able to get out in the country; to exercise in a way that was not at all a strain on my left hip; and mostly to have the freedom to move my body and do something besides my hobble-walk – by comparison to my walk, my rate of speed on my C80 is Gazelle-like. I downloaded an app called Cyclemeter, the cycling equivalent to the Nike Run app I used when running. And yet, the cyclemeter app is quite sophisticated; it shows a full map of the route taken, elevation changes, temperature etc. For example, here is the data and map from a ride I did on 24 October 2021:
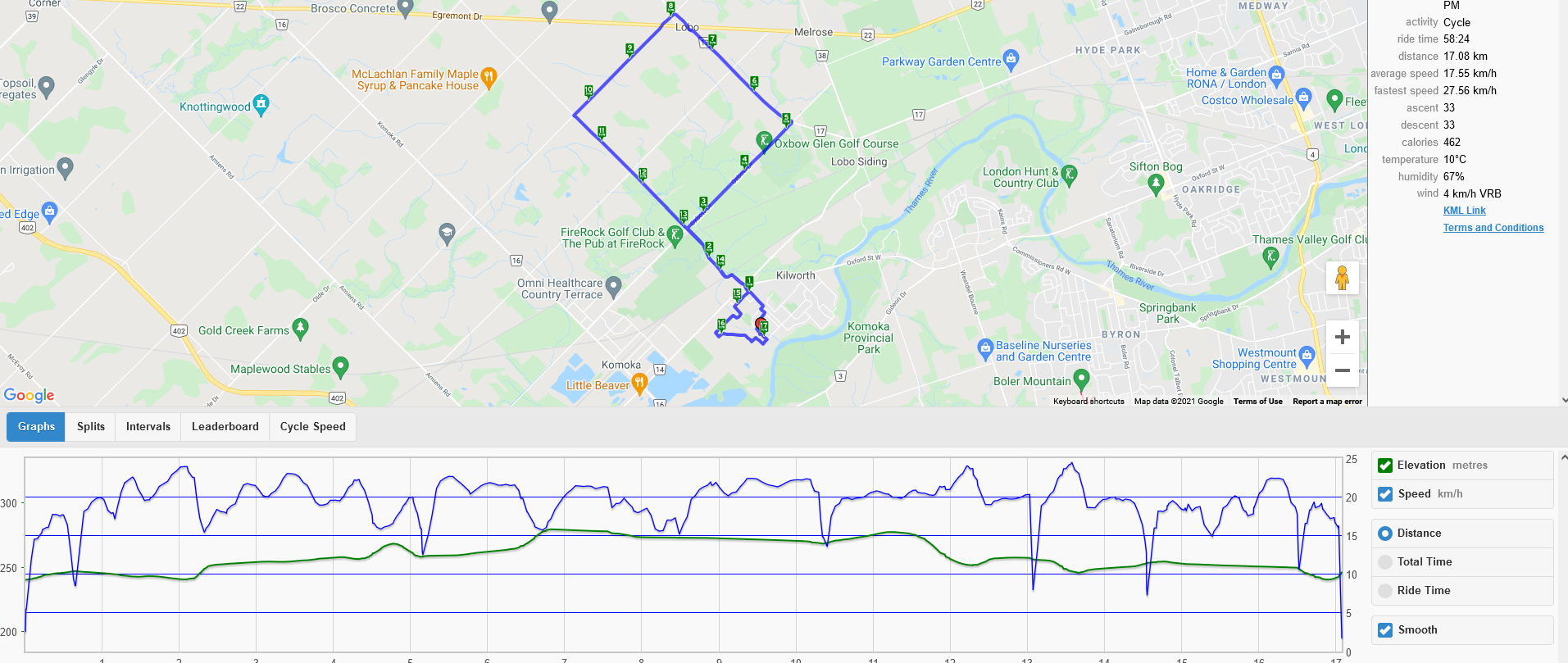
My interest in the new app is just to track routes and note distances for each ride. Since late June and as of early November 2021, I logged almost 2000 km. I don’t get the same cardio workout that I did running and I expect most of that is because I use the e-assist a lot to ensure ease of pressure on my hip. Finding and exploring new routes, using country roads north and south of our home, and just riding are fun, again, unanticipated when one is wedded to running. I can climb any hill with minimal effort using the e-assist. I do not relish going downhill at any kind of speed = equal to or greater than 20 km/hour, always applying slight brake pressure when I do downhills to avoid any risk of falling. The bike is a step-through, that is, no crossbar so it’s easy for me to mount. And I taught myself to make certain the left pedal was at the bottom of its arc if I anticipate stopping, ensuring I could use my right leg to take my body weight in stepping down to the ground at the stop.
A few months before I purchased my Gazelle, in early April of 2021, as my recognition of my needs for exercise given my osteoarthritis and limited mobility issues became more apparent, my intuition was that the ideal cardio exercise system would be rowing on an ergometer – an erg. I had owned one years ago and of all the stationary exercise equipment I have ever tried, I found it to be the most challenging and interesting. So I contacted a former student who had become one of Western’s rowing coaches; rowers use rowing ergs as training devices in the off season. His advice was to get a good one, a Concept 2 and he warned that because of Covid and the inclination of folks to create home gyms with home exercise equipment, they were really difficult to get. I searched online and contacted Rogue Fitness Canada who, in turn, were able to order shipments direct from the American-based Concept 2 manufacturer with no duty charge and free delivery. It came via UPS within 2 weeks in this container:

Assembly was pretty simple via specific, easy-to-follow instructions. Within an hour, it was row-ready:

We moved it to a better location near the window for both the view and fan-blown fresh air and installed a mat for stability, no rug wear, and to catch sweat:
 Daily, following our dog walks – Jazzi and Tiso were so patient and accommodating to my slowed pace – I exercised on the erg, starting at 5 minutes and working my way up to rides of 30-35 minutes. With noise-cancelling ear-phones connected to my ipod, and having watched instructional youtube videos, I thoroughly enjoyed rowing…even added a form-fitting, padded seat to the sliding seat-device for extra comfort. Within a couple of months, I found my range of hip motion decreased and getting full range of motion on the erg was restricted. Also, I was a bit hip-sore after some rowing workouts. By then, I had started using my e-bike with no impact on range of motion so I made the decision to purchase the same rower-erg brand, Concept 2 stationary bike, now sitting proudly beside the treadmill we have owned for years:
Daily, following our dog walks – Jazzi and Tiso were so patient and accommodating to my slowed pace – I exercised on the erg, starting at 5 minutes and working my way up to rides of 30-35 minutes. With noise-cancelling ear-phones connected to my ipod, and having watched instructional youtube videos, I thoroughly enjoyed rowing…even added a form-fitting, padded seat to the sliding seat-device for extra comfort. Within a couple of months, I found my range of hip motion decreased and getting full range of motion on the erg was restricted. Also, I was a bit hip-sore after some rowing workouts. By then, I had started using my e-bike with no impact on range of motion so I made the decision to purchase the same rower-erg brand, Concept 2 stationary bike, now sitting proudly beside the treadmill we have owned for years:
 I have never, ever enjoyed riding stationary bikes when I needed to do so while rehabilitating from some running injury. This one is different, perhaps because of its similarity to the rowing erg re their digital, battery-operated performance monitor, the PM5, mounted on the front of each machine within eyesight and easy reach for progamming and viewing:
I have never, ever enjoyed riding stationary bikes when I needed to do so while rehabilitating from some running injury. This one is different, perhaps because of its similarity to the rowing erg re their digital, battery-operated performance monitor, the PM5, mounted on the front of each machine within eyesight and easy reach for progamming and viewing: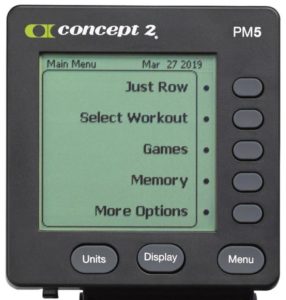 The PM5 on the bike erg says, “Just Ride” at the top and both are linked to a website where you can record daily rowing/riding, get workout hints, do challenging events and who knows what else; my interest is more in getting a good cardio workout and one that produces a good workout sweat, the latter something I really miss from running. The little plastic hook above each PM5 in the ergometer images above – best seen in the bike erg picture – took me a while to discern their utility; turns out, it’s a pliable holder for a cell phone inserted horizontally. All three of my machines have become important in my daily activity repertoire; should slippery, winter conditions happen, I can use the treadmill for walking, the latter activity regarded by many as the best exercise following hip replacement surgery. Thus, once a runner, I am now a cycologist, perhaps even an ergologist, at the very least, a gazelle (my e-bike brand) of sorts.
The PM5 on the bike erg says, “Just Ride” at the top and both are linked to a website where you can record daily rowing/riding, get workout hints, do challenging events and who knows what else; my interest is more in getting a good cardio workout and one that produces a good workout sweat, the latter something I really miss from running. The little plastic hook above each PM5 in the ergometer images above – best seen in the bike erg picture – took me a while to discern their utility; turns out, it’s a pliable holder for a cell phone inserted horizontally. All three of my machines have become important in my daily activity repertoire; should slippery, winter conditions happen, I can use the treadmill for walking, the latter activity regarded by many as the best exercise following hip replacement surgery. Thus, once a runner, I am now a cycologist, perhaps even an ergologist, at the very least, a gazelle (my e-bike brand) of sorts.
Very happily, as I start to ‘pen’ this blog on 14 November 2021, I can record that I was able to get full left hip replacement surgery on November 9th at Women’s College Hospital in Toronto. On 28 October, I received this email:
Hi Don,
I can schedule your surgery on November 9th at Women’s College Hospital – will this work for you? As this is short notice, I have a tight deadline of getting the paperwork in. if you could let me know as soon as possible, that would be appreciated.
Thank you!!
Simone Wynia, Medical Administrative Assistant, Dr. Michael Zywiel
Would that work for me??!! Truth is, I’d have crawled to Toronto for the surgery. The very earliest I thought I would be eligible for the surgery was the end of November and every wait-list on which I registered predicted sometime in February, likely later. I happened to be on my computer when Simone’s email arrived; within seconds, I emailed and called her office to accept. Right after that, ecstatic with the news, I called Jen who was in Georgetown with her mom. She was thrilled.
The operation was at 8:00 in the morning, first one of the day, though we did not know the time until the day before the surgery. Jen and I did a lot of planning compacted into a very few days before the 9th and a time period compacted by a family member’s surgery a week before the October 28th notification. We decided it was safest and best plan to book 2 nights at the Holiday Inn near Women’s College hospital; it would give us timing flexibility and give Jen a place to be during the operation and recovery given she was not allowed to accompany me into the hospital. Our only reluctance in doing so, was being in such a public place just as Covid’s 4th wave was still in bloom and we would be in close human contact. So, we purchased a high quality HEPA air purifier, determined to keep our hotel ‘suite’ as clean as possible, after verifying that we could book a room where windows could open to have fresh air. Jen also planned and prepared and brought all our food so we could minimize going out of our room and/or into other areas of contact. We also rented a driver service, a large SUV. The vehicle and its driver too were a high contact risk for us; however, we felt it the best way to avoid Toronto traffic and give me greater leg room. Drivers going there and coming back were very respectful about wearing a mask, even consenting to using N95 masks we supplied for them.
We checked into the hotel, 500 meters from the hospital by late afternoon on the 8th. Both of us noticed the haphazard approach to masking and distancing in downtown Toronto and in the hotel. Chicken stir fry, one of my favourites was the pre surgery dinner with no food or drink after midnight. We slept reasonably well, up at 5:15 and at the hospital via cab by 6:00 AM, as instructed. We had to wait for the Covid security folks to open the front doors and when they did, a few minutes after our arrival, Jen went back to the hotel administering lots of ‘masked’ kisses, big hugs, and saying, “you got this.”
Admission was seamless: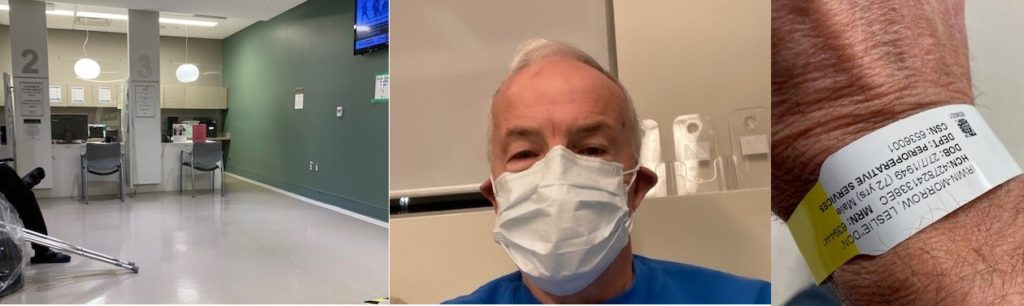 8th Floor admitting area with crutches for post-op; double-masked (N95 & medical) patient, my last image with both hips intact; hospital ID-braceleted for the surgery
8th Floor admitting area with crutches for post-op; double-masked (N95 & medical) patient, my last image with both hips intact; hospital ID-braceleted for the surgery
Within minutes, I was taken into change area, was given the lovely hospital gown, and told only clothing I could wear was my socks – my beloved Thorlos – because of how cold it would be in the operating room. All my belongings were put in a locker, #17, a good number, one with which I felt very comfortable would yield my clothing etc post-op. Very soon, a nurse called me into the pre-operating area and did my vitals – very high systolic blood pressure (190). “Was I nervous,” she asked. Indeed, I was very nervous and had the same BP reaction just before my rotator cuff (shoulder) surgery in 2015. My BP is normally 125/85 pretty consistently. She administered me a few pills – what they were, I do not recall. Then she walked me a ways down the hall to the nerve-block, pre-op preparatory area.
This room was the last phase before the operation. All manner of hospital personnel seemed to swarm around me, flitting in to ask a question or two – date of birth, what surgery was I having (Dr Zywiel had already ‘autographed’ my left hip, a source of great comfort), was I allergic to anything, where was I, and what was today’s date. After that, someone put a port into the crux of my left elbow while someone else put heart monitor chest leads on me. There seemed to be 2 or 3 different anesthetists who introduced themselves to me and told me I would be getting an epidural nerve block – did I know that…yes I did. Dr Zywiel appeared again because my signature did not show up on the emailed permission to operate form so I needed to re-sign with him present. Finally, I was asked to sit on the edge of the cot-bed and a portable table that looked like an airport sitting-massage unit was wheeled up to me. They put a hair net or light head covering on me, asked me to lean into the headrest, arms up on the unit’s shelf. Someone started to swab my lower back, presumably with antiseptic for the epidural needle. Curiously to me now, is that swabbing is the last thing I remember – I have no memory of the epidural needle, no recall of being wheeled to the operating room. The next thing of which I was conscious was waking up here: 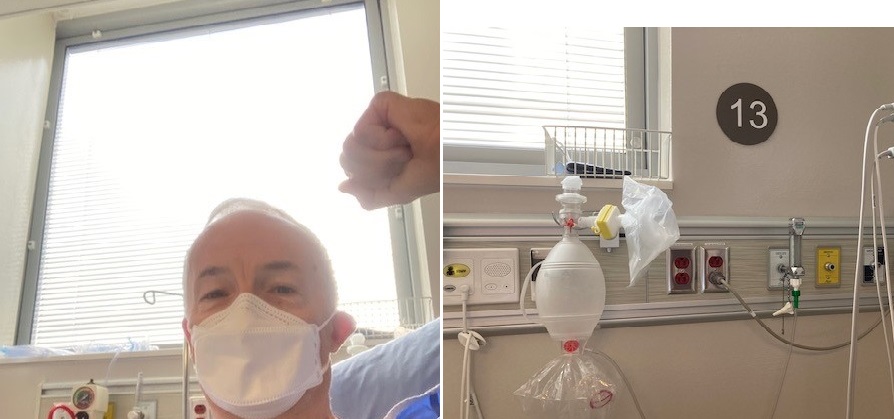 This was the recovery room; the fact that it was area # 13 didn’t seem to matter at the time. Serena, a student nurse was at the foot of the bed intent on working at her portable computer. She was delightful, very caring, kind, and even went through my retrieved bag to get my cell phone in order for me to send the picture to Jen and call her. Dr Zywiel had already called Jen to tell her everything went very well. The surgery is a 90-minute process, quite stunning to me when considering they take out a piece of hip bone (primarily the head of the femur) and then put in a whole new, artificial hip after ‘cleaning up” any lingering osteoarthritic bone around the acetabulum, the socket of the hip. I knew the basic idea of this, Direct Anterior Approach (DAA) to total hip replacement but I did not want to know any details pre-surgery. A few days after my operation, I watched this full video of the DAA, selecting it because the surgeon explained to a colleague everything he was doing and the reasons for each step. Out of curiosity, when Dr Zywiel came into the recovery room to check on me, I asked if he had a picture of the head of my femur (thigh) bone that he extracted. Immediately, he pulled out his cell phone and showed me the image. I asked him to send it to me. I have inserted the image as a link wanting to respect the fact that some folks might not want to see it; so readers can click on don’s femur head by choice to see the image if you wish. Schematically, this is what the interior of my hip now resembles:
This was the recovery room; the fact that it was area # 13 didn’t seem to matter at the time. Serena, a student nurse was at the foot of the bed intent on working at her portable computer. She was delightful, very caring, kind, and even went through my retrieved bag to get my cell phone in order for me to send the picture to Jen and call her. Dr Zywiel had already called Jen to tell her everything went very well. The surgery is a 90-minute process, quite stunning to me when considering they take out a piece of hip bone (primarily the head of the femur) and then put in a whole new, artificial hip after ‘cleaning up” any lingering osteoarthritic bone around the acetabulum, the socket of the hip. I knew the basic idea of this, Direct Anterior Approach (DAA) to total hip replacement but I did not want to know any details pre-surgery. A few days after my operation, I watched this full video of the DAA, selecting it because the surgeon explained to a colleague everything he was doing and the reasons for each step. Out of curiosity, when Dr Zywiel came into the recovery room to check on me, I asked if he had a picture of the head of my femur (thigh) bone that he extracted. Immediately, he pulled out his cell phone and showed me the image. I asked him to send it to me. I have inserted the image as a link wanting to respect the fact that some folks might not want to see it; so readers can click on don’s femur head by choice to see the image if you wish. Schematically, this is what the interior of my hip now resembles: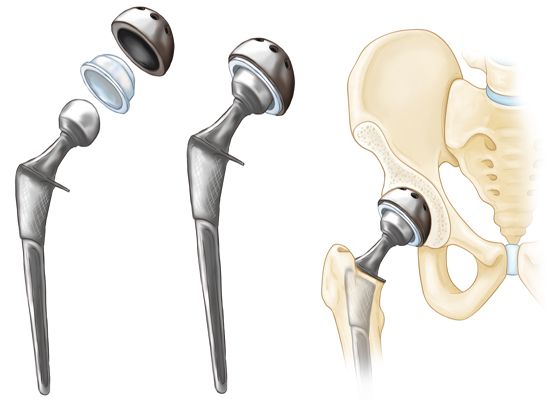 Quite a precision-engineered device and sophisticated procedure is this, from my perspective. Imagine being able to replace that with which I was born with something so ingeniously artificial and so superbly functional! My actual hip replacement, that is, in my hip can be seen here:
Quite a precision-engineered device and sophisticated procedure is this, from my perspective. Imagine being able to replace that with which I was born with something so ingeniously artificial and so superbly functional! My actual hip replacement, that is, in my hip can be seen here:

I was unaware that there was an anchor screw until I saw this image at Toronto General Hospital at my 16-day post-op appointment on 25 November with Dr Zywiel – makes sense that they and I don’t want the titanium cup slipping around inside my hip bone. Two other x-ray images illumine the intricacies of this operation. This first one, immediately below shows how centred the anchor stem is inside my femur. When the medical team at my follow-up appointment saw this x-ray, I was delighted that the first person said, “perfect” and then brought in others to see the image. I really did not want to have any surgical adjustments.

This x-ray image below was taken with me lying on my side so that the image looks like it is flat; I guess they wanted to see the stem-placement from a lateral view:

Incredible to me that they do all that in less than 90 minutes of surgical time. And, the incision – your choice to view it by clicking on the green, bold-ed words – is only about 4 inches long, no staples, dissolving sutures. Equally stunning, my legs are exactly the same length post-op. I was in recovery for about 3 hours. It took an hour or so for me to start to be able to feel my legs, the sensation returned gradually. I texted Jen a lot, was visited by a pharmacist who went through a cornucopia of pills I need to take, from the opioid pain reliever hydromorphone through to acetaminophen and Celbrex to stool softeners etc. She gave me a full printout of all the drugs and their instructions and told me Jen had been notified to pick the prescription/s up from the Rexall pharmacy located on the main floor of Women’s College. Apparently, I could have been discharged before noon; however, the last step in the process was that a physio, Hari needed to assess my ability to move with a walker and on crutches. Hari was stuck in a meeting for a long time and apologized profusely when he showed up. As soon as he arrived, he helped me get up, affixed crutches under my armpits and walked beside me down the hall about 50 feet, stopping once to switch to a 2-wheeled walker and subsequently for a bathroom break. Then, he had me, crutch-assisted, climb a fabricated set of 3-stairs, up and down, being careful to stay close to and instruct me. In the week before surgery, I had rented a 2-wheeled walker, a cane, and crutches and I practised on all of the devices so that I could get used to them and so that our dogs would be aware of them too. Passing all the mobility tests, Serena helped me pack up my backpack including all drug and post-op information and I was wheel-chaired down to the main floor entrance where Jen was waiting with our SUV driver. She had packed up everything at the Holiday Inn where the driver picked her up to come to Women’s College. Vividly, I remember the gush of emotion seeing Jen again; it was hard not having her in the hospital with me. We were back at our home by 3:30 that afternoon.
I wish I could say that the saga from this point became one of recovery at home. The # 13 in the recovery room had not come to its foreshadowed fruition just yet. The morning after my surgery, we were up early, took my time getting up, and escorted by Jen, using my walker, we went out to the kitchen. I started to get cream out of the fridge for my coffee and felt faint. I sat down on one of the bar-stools at our kitchen island and passed out. The next thing I remember was Jen poking me and saying, ‘don, wake up, don, wake up’ and as I came to, I realized she was on the phone calling 9-1-1 and an ambulance had been dispatched. To this day, we think it was a vasovagal event, medially termed “vasovagal (or neurocardiogenic) syncope” when you faint because your body overreacts to certain situations. The vasovagal syncope trigger causes your heart rate and blood pressure to drop suddenly. I have had it happen to me before, getting up too fast from bed but it hadn’t happened for a long time. The trigger was likely some combination of post-surgical stress, dehydration, the cocktail of medications – who knows. In this instance, I also had stopped breathing. Jen knew exactly what to do – get me to be lying down on the floor; however, my legs were wedged under the island counter and pinned by the vertical side-piece. And she was concerned about damaging the incision and/or new hip. So, she said she squirted apple juice from a juice box that caused me to choke so she administered the heimlich maneuver and that’s when I came back to consciousness, spewing apple juice as I did so. I cannot begin to imagine the trauma impact on Jen and her quick-thinking saved my life.
Within minutes, it seemed to me, Kristen and Alex, the ambulance paramedics arrived. It felt like being in a fog to me, barely discerning Jen re-telling the events, giving them info about my surgery and so forth. They did my vitals and advised that the safest thing to do would be to take me to the Emergency Department at University Hospital. I suspect I was reluctant but relied on Jen and the paramedics. While they got me into the ambulance, Jen got me a full set of clean clothes, my cell phone, all my meds, and some bran muffins. Kristen stayed with me in the back of the ambulance and kept talking with me to keep me conscious. I don’t think Alex drove any faster than usual; however, it seemed to me he made a lot of turns and with no window in the ambulance, I started to heave. Kristen asked if I wanted an injection for my nausea; I did, she administered it, stopped the nausea but my shoulder still feels slightly sore from where/how she injected the needle in my shoulder. Regardless, their advice to go to the hospital was one of two instances of medical intuition that were in my favour that day (Jen’s quick-thinking was likely a third).
I was admitted very quickly, owing to the time of day, maybe 6:45 am or so by then. The paramedics wheeled me into an examining room in the ED, transferred me to a hospital bed, wished me well and left. I hope I thanked them.

Me, in the ED sporting a shielded University Hospital mask
In a matter of minutes, a Dr Lin arrived at my bedside, introduced himself and told me he knew about my case. Dr Lin was very kind, very attentive. He knew what had happened, reviewed it with me and said he was 95% convinced it was merely vasovagal syncope. To be sure, they would do some repeated blood work and to be doubly sure, he would order a lung CAT scan. Dr Lin said he just had a hunch it would be an extra measure of safety. At the time, I didn’t know what was the purpose of the scan but trusted Dr Lin’s judgment.
I was given ice-water to drink but told not to eat because of the repeated blood tests that would be done. Hungrily, I stared repeatedly at the bran muffins in the Ziploc bag on my bedside table – perhaps the muffins would sneak in by osmosis without anyone knowing, I thought. During the morning, I had blood taken at least twice and I had someone come in and put more monitor leads on my body than I had ever seen on television shows…at least a dozen, maybe more. It was some advanced electrocardiogram process that allowed them to record heart functions over an extended period of time. Turns out, all blood tests normal, all heart monitoring produced normal results. At mid-morning, I was wheeled in the bed to the CAT scan area, transferred to the scan-bed, and asked if I had ever had some kind of dye injected into me (I had not). At some point the technician must have hooked me up to the dye-injection process through a portal in the back of my hand. She asked me to raise my arms and place them elbows-bent behind my head and then just follow the audio instructions. Either the bed I was on or the CAT scan, circular machine moved until my chest was under it. “Breathe out. Take a deep breath. Stop breathing. Breathe” were the computer-voice, recorded instructions given to me 4 or 5 times as i was moved in and out of the machine’s circumference. During a couple of times, I could feel and kind of hear the injected dye going into my hand, a weird but not painful sensation. The whole CAT scan process took less than 5 minutes. I was transferred back to my bed and wheeled back to my room in the heart of the ED; on the way, I was told it takes a long time to get CAT scan results, perhaps a couple of hours or more.
I spent those hours texting and/or calling Jen, can’t remember if or when I did either/both. She had contacted our friends Clive and Brynah who live near the hospital and Clive offered to take me home when I was done. At some point, perhaps from Dr Lin, I was told they were wanting to make sure there was no clot in my lung. From all the research I had done about full hip replacement surgery as well as from info on the pre-surgery forms, I was aware that blood clots happened in less than 1% of these operations – it is one of the risks. Finally around 12:30, I think, a doctor came in – cannot remember his name now – told me Dr Lin was off-shift and that they had the CAT scan results. Before he told me the results, he said it was fortunate that Dr Lin had ordered the scan; the new doctor said I had no presenting symptoms – like problems breathing or chest pains – and he said it was unlikely most other doctors would have requested the scan. Turns out, I have a small pulmonary embolism in the upper right quadrant of one lung, specifically from the radiologist’s report:
Study is positive for pulmonary embolism with a single occlusive filling defect
in a segmental branch of the right upper lobe. No associated pulmonary infarct
or hemorrhage. Overall clot burden is low
The only thing uplifting about the wording above, to me, is “overall clot burden is low” – surely a good finding! I have access to the scans and have no way of reading the images but cool to see my chest internally, distorted though the angle of this view:

Somewhere in there the little “clot burden” lurks! There is no way of knowing if it had been in situ for some time or if it was coincident with my hip surgery the day before. Embolisms or clots are not to be dismissed. I was given a massive dose of some potent anti-coagulant – Fragmin, 17,000 units, as it turns out – administered hypodermically into my abdomen and told I was to go immediately to Victoria Hospital in south London to see Dr Kovacs, a hematologist who had been called re my CAT scan results and who ordered the injection and who asked to see me right away.
At Victoria hospital, Clive and I were greeted by a line-up of some 75 people waiting to go through Covid pre-screening and the line was barely moving to get into ‘E’ Wing of the facility.
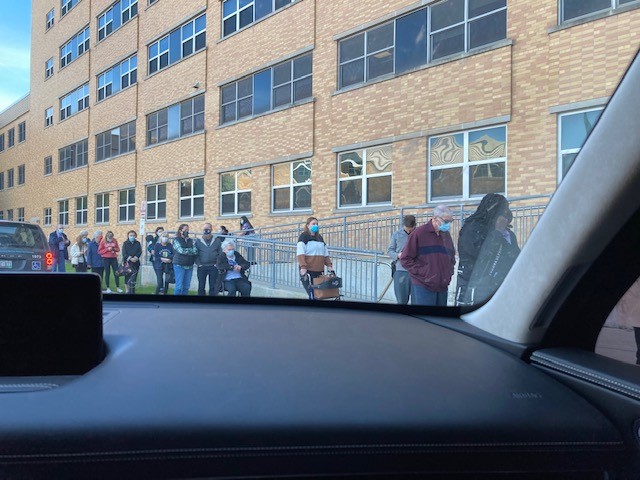
I remember as we pulled up to the building and as I took the picture above from Clive’s vehicle, that this was the facility in which my father had spent a lot of his hospital time many years ago. In fact, in retrospect, it was in this hospital where dad had his left leg amputated below the knee owing to the ravages of smoking and the shut down of blood circulation in his extremity. How ironic I was here following a left leg hip replacement. We decided that Clive would get a wheelchair and see if we could get near the door via the access ramp. We did and just as we got there, a security person opened the doors; I told him we were told by UH doctors to see Dr Kovacs “right away” (we actually were told that) and he motioned us to the screening area. Within minutes, I was in the elevator on the way to the 5th floor, wheeled by hospital staff. Receptionist desk person on that floor said Clive, my support person could come up so I texted him and he joined me in an examining room. Dr To, a resident with Dr Kovacs did my intake, a full assessment including vitals. His conclusions, verified by Dr Kovacs moments later were:
ASSESSMENT AND PLAN: In summary, this is a previously healthy 72-year-old male with a
segmental pulmonary embolism diagnosed today, postoperative day 1 from a left total hip
arthroplasty. This would be considered a provoked PE. It is not entirely convincing that his
syncopal episode could be explained by his PE given that it is relatively small burden; however,
now that it has been discovered, we will need to treat it. We discussed the following plan:
1. With regards to anticoagulation, he does require anticoagulation for 3 months. We
discussed options and introduced the COBRRA study. He consented to participation in the
COBRRA study and was randomized to apixaban. He was prescribed apixaban 10 mg b.i.d. for
7 days, followed by 5 mg b.i.d. He was counselled regarding risk of major bleeding of about 1%
to 2% per year. He was counselled that he should seek urgent medical attention for any major
bleeding or significant symptoms of chest pain or shortness of breath or any worsening
syncope.
2. He was counselled that he should participate in any and all recommendations as per his
orthopaedic surgeon. There should be no activity restrictions related to his rehab from the hip
surgery from our perspective.
3. We did ask him to stop his Aspirin today as this was prescribed from the point of view of DVT
prophylaxis postoperative. This is not a preexisting medication for him.
4. We will see him back in followup in 2 weeks’ time and then 3 months’ time, or sooner should
the need arise.
The sentence in the first italicized paragraph above – “It is not entirely convincing…” – is the one that suggests my fainting episode at home was not embolism-provoked because of its small size; nevertheless, it was important to deal with it. To me, this whole day seemed like an ongoing confluence of being in slow-motion time, kind of hovering and observing what was going on and, at the same time, it felt like a whirlwind of activity happening in a fog of gattling-like events, okay, Jen has 9-1-1 on the phone, okay, I’m in an ambulance, okay, blood tests, okay, CAT scan, okay off to Victoria hospital. I had no control over any of the events and seemed to trust that the universe would unfold exactly as it should, or, as Clive often says, making the same statement with this addendum…exactly as it should…or else it won’t. Seems like it did unfold, one way or the other, and that I was wilfully in the hands of allopathic medicine.
I cannot begin to imagine the impact of all of these events on Jen and I so regret and detest that I put her through everything that happened. Jen is an incredible human being, one with whom I am so privileged to share life. Were there any way to retract or even ease the trauma she experienced on November 10th, I would gladly exact that remedy. She is so incredibly not just smart but so insightful. For example, I know she and Dr Zywiel were in contact by phone and by email in her effort to make sure everyone knew what was going on and if there were anything at all we should know from Dr Zywiel. His preference would have been a more mild or prophylactic anticoagulant than Apixaban; we chose to rely on the hematologist on the advice of every medical person in our hemisphere of advisors. There is a wonderful symbiosis of care and love between Jen and me that I just cherish.
Clive drove me home from Victoria hospital, kind and gracious as is his way always. My recall is he drove very slowly and carefully that day, likely sensitive to any impact of movement on my hip (and/or my lung). As the days have unfolded since that day, I have had no known or felt repercussions of the high dose anticoagulant, Apixaban. Each day, it seems like post-op recovery has been going really well. Within a couple of days, Sherrill, Jen’s mom came to stay with us to help Jen out; she is a treat just to be with and she has been so incredible in supporting us both, always on the go doing something around the house. She and Jen have such a close relationship and I know it is so comforting to Jen to have her mother with us. My whole focus for about 7 days was on rehabilitation – my human ‘doing’ way of being was put on hold.
For a few days, I went everywhere with my two-wheeled walker, using crutches for our stairs always accompanied and guided by Jen. Going downstairs, positioning herself at the bottom of the staircase, she would chant, “bend, crutch, new (surgical, left leg)…” and going upstairs, “good (leg), crutch, new…” til eventually we made them into Russian-sounding words, ‘bendcrutchnew,’ for example. We used the walker when I was seated anywhere as a deterrent to Jazzi and Tiso jumping up on me, either onto the incision area or scratching me inadvertently, the latter a potential concern re bleeding and/or bruising. They both seemed to ‘get it’ and know that something is different and to be careful around me, strange as that might sound to non-dog-owner folks. Gradually, I transitioned to crutches for walking then to my cane. I have walked outside with all 3 assistive devices and now, as of November 20th, 11 days since surgery, walking without any device. This video of me free-walking was taken on Sunday the 21st. As device-free as that video reveals, it is taking me time and effort not to ‘baby’ my left leg – still can’t quite convince myself it’s not going to hurt when I put full weight on it and take a full stride.
I am so grateful, first of all to Jen, and then to Sherrill, and then to modern medicine, and then to all the folks, family, and friends who have sent their well-wishes along with so many offers to help us out in any way at all. 12 days later, the vasovagal syncope event and its aftermath seem surreal. At the same time, I now sport a medical reminder with a Medic-alert bracelet on its way:

I started this Cycologist blog talking about my transition to an electric-assist bike because of hip osteoarthritis uprooting my running life-style. All of the adaptations I’ve implemented, from the e-bike to the rowing erg to the bike erg have served my yen and need for physical activity, physically and psychologically. And as of November 9th, a magician (Dr Zywiel – I acknowledged him personally with this noun; he “doubted” it) has given me a gift, an internal assistive device in the form of an artitifical hip. I will not take this gift for granted as I move through all the physiotherapy I am now doing. Nor will I forget the events of November 10th, the “little clot burden,” the vasovagal syncope that triggered the clot discovery, and more, much more that anything, Jen’s love and care for me, my care-ologist in all of this. It has been, for both of us, quite a ‘ride.’ I tumble home to my devices, external and internal, and to all those people and events who assisted me to be where I am today.
4 February 2023. Almost 15 months have passed since I wrote the blog above. Re-reading it now, the evens surrounding my surgery feel surreal to me, as though the surgery and after-math were all a dream-state. I have absolutely no movement issues with my left hip; it feels like it always did pre osteoarthritis. In late November 2022, one-year post-op, I had a follow-up phone-call session with Dr Zywiel, an event scheduled when I left my in-person visit with him at Toronto General Hospital some 3 weeks after my surgery. In the one-year follow-up, he just asked how I was doing, if there were any issues etc. One question he asked seemed odd to me – “do you sometimes forget you have an artificial hip?,” he inquired. After reflection, I told him I never thought of it like that. For me, I am just so grateful to be able to walk normally and be pain-free. I can’t “feel” the artificial hip and the scar is fading and is only about 4 inches long. I wonder now if his question came from someone who has not had hip replacement surgery and he was just curious about how patients perceive having an artificial hip.
24 July 2023 Addendum. It is now 2 years since I purchased my Gazelle Ultimate C80 e-bike. In short, I just love riding it!! About 3 weeks ago, my kilometer marker reached this milestone:

5000 km is equivalent to one trip across Canada, coast-to-coast. Significantly, I achieved this, not as a specific goal…more just one that was noticed. It happened at the corner of McEvoy and Scotchmere roads on one my longer riding routes (48 km round-trip) and happened right in front of the Caradoc Presbyterian Church

My McCullough (my mother’s family) ancestors, staunch Presbyterians, would be proud. This corner, right at the front steps of the church is one of my rest-to-hydrate stops on my rides in the countryside north of our home. There is a freedom and pure enjoyment in riding my e-bike, something I had not anticipated. It is a gentle exhilaration traversing country roads, paved and unpaved, testing my stamina with lower gears, using the electric assist – Eco~Tour~Sport~Turbo, the four assist levels, low to high – whenever I want to and/or need to do so.
For a full description of my life-long fascination with ‘the wheel,’ see my June 2022 blog, Riding History.
